Hank Fall 2014
See the whole issueCuriosity Leads to Better Service
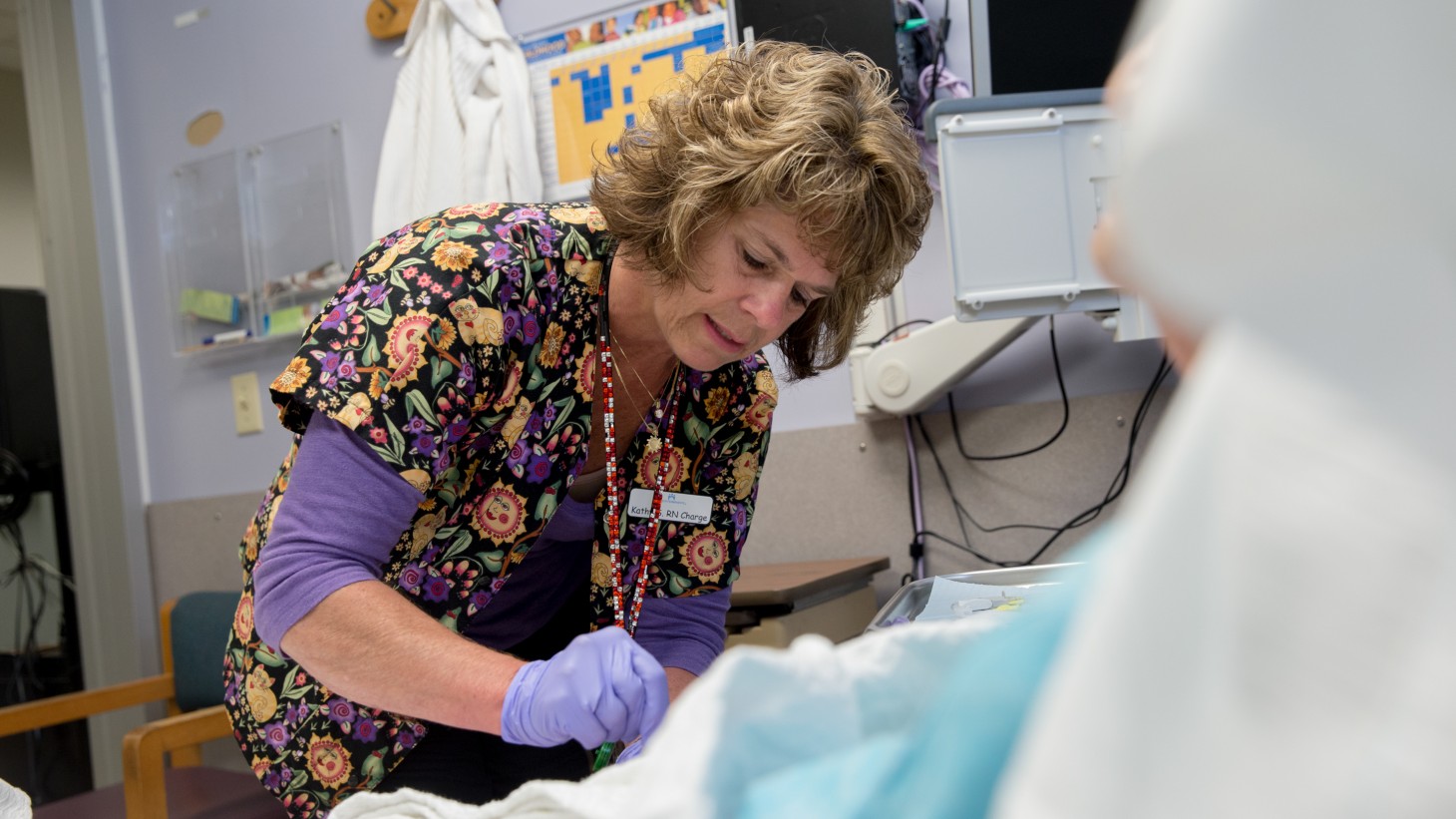
RN Kathy Stafford, a member of the Oregon Nurses Association
Adopting a best practice from another team, an Infusion Center improves care for patients
The word “rapid” stopped Kathy Stafford, RN, and made her ask more questions.
Stafford, the UBT co-lead and charge nurse for the Regional Infusion Center in the Northwest, had been reading an email from a Colorado colleague. The colleague wondered whether the center was using a new protocol for Remicade, an infusion drug prescribed for such diseases as Crohn’s, rheumatoid arthritis and psoriatric arthritis. The Colorado infusion center was trying a new “rapid” Remicade delivery method and looking to see what the experience of others had been.
The Northwest still was using the standard method, and Stafford, a member of the Oregon Nurses Association, was instantly curious. A regular Remicade infusion takes 3½ hours—three hours for the delivery of the drug, and then, to be sure there are no adverse effects, the patient has to wait 30 minutes before being discharged. The new protocol reduces that to a total of 1½ hours.
The gift of time
“If there is anything we can do to speed up infusions for our patients,” Stafford says, “it would be a service to them and, at the same time, save the organization money.”
In short, Stafford was putting the patient at the center of her decision making, bringing the Value Compass to life. The rapid Remicade protocol improves the patient’s care experience and improves service, quality, affordability and staff satisfaction:
- Patients spend less time in the clinic, since both the drug administration time and post-infusion wait time are reduced.
- Because patients are spending less time in the clinic, more patients can be seen. Up to 16 hours of patient chair time could be opened up every day.
- Because the clinic can accommodate more patients, fewer patients will be redirected for treatment in the Emergency department or at the regional Oncology department, improving those departments’ ability to serve their primary patients.
“Any chance we have to be more effective is worth it, so we can spend more time with our patients,” Stafford says.
Making it happen
Following up on the initial email inquiry, Stafford learned the evidence-based practice already was being used in Colorado and the California regions. She and Greg Frazier, the assistant department administrator and UBT management co-lead, pushed ahead with getting the protocol approved for use in the Northwest, benefitting all the region’s eligible patients.
“There was no stopping Kathy,” Frazier says. “She knew who to talk to in the organization and how to move things along….
“Our team is always looking at how to do things better, and to take care of the patient the best we can,” Frazier continues. Noting that the infusion team is highly motivated and self-directed, he offered words of encouragement to those who see an opportunity they want to pursue.
“Don’t turn away from a challenge. Ask questions,” he says. “It may not work, but look into it first before you discount it.”
Stafford credits the team for getting the new protocol approved so quickly, despite a complex approval process that included meetings with both physicians and pharmacists.
“Without the enthusiasm and involvement of the infusion RN team, this would not have gone as smoothly,” she says. “We found out about the protocol in March and we began implementation in May. That’s pretty fast.”
